
Executive Summary
Healthcare organizations generate over 50 petabytes of data every year, spanning clinical notes, lab tests, imaging files, sensor readings, genomic profiles, and even financial data. Yet, an estimated 97% of this information remains unused [1]. Unlocking its potential could dramatically improve the quality and timeliness of medical care.
Generative AI is emerging as a catalyst for change. In clinical research, it has already accelerated report timelines by up to 40% and achieved accuracy rates above 98%, reducing errors compared to human-only drafts [2]. These same capabilities, automating text generation, structuring data, and cutting repetitive work, are increasingly relevant for everyday clinical documentation.
Beyond trials, AI-driven workflows can reduce operational costs and speed up decision-making across healthcare settings [3]. At the market level, the global healthcare business intelligence sector, valued at USD 9.92 billion in 2024, is projected to reach USD 31.8 billion by 2033, expanding at a 13.9% CAGR. This growth reflects the rising demand for data-driven decision-making and stronger adoption of electronic health records (EHRs) [4].
Together, these forces are shifting healthcare from fragmented, underutilized data pools to AI-enabled platforms that transform clinical conversations and records into actionable insights.
This blog explores how natural language processing (NLP) and AI can structure clinical conversations, reduce documentation burden, and power healthcare data analytics platforms that drive measurable improvements in safety, efficiency, and patient outcomes.
I. Why Structured Clinical Data Matters
Most patient interactions generate free-text notes, dictated summaries, or transcripts that contain valuable clinical information but remain largely unstructured. Without standardized data, even the most advanced analytics or AI systems cannot effectively interpret or act on these insights.
The absence of structure makes it difficult to:
- Benchmark outcomes or identify performance gaps
- Support population health programs and predictive models
- Monitor safety metrics and compliance indicators in real time
Structured clinical data establishes the groundwork for AI readiness. When healthcare organizations record and organize information using consistent coding standards and measurable outcomes, it becomes possible to analyze trends, automate routine reporting, and drive continuous improvement across care settings
II. How NLP Extracts Meaning from Clinical Conversations
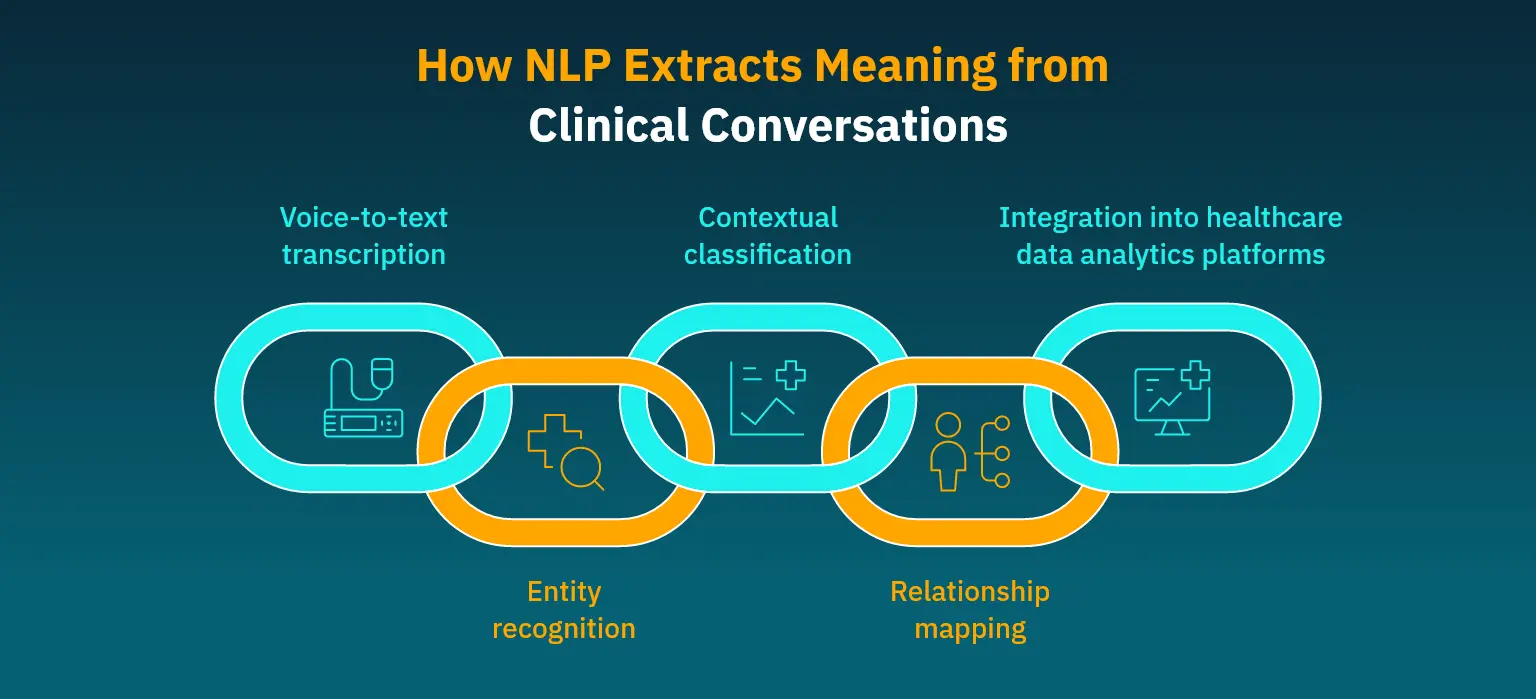
Modern NLP models do more than transcribe audio into text. They are capable of interpreting the nuances of physician-patient interactions and structuring that information for downstream analytics. This process is critical because the majority of clinical documentation still originates as free-text notes or dictated conversations.
Here’s a step-by-step flow of how conversation becomes structured insight:
- Voice-to-text transcription
High-accuracy medical speech recognition engines capture physician and patient dialogue. Unlike generic transcription tools, medical-grade models are trained on clinical vocabularies, abbreviations, and context-specific phrasing. This reduces common misinterpretations of terms like “COPD” or “MI.”
- Entity recognition
NLP algorithms identify and tag medically relevant entities such as diagnoses, lab values, drug names, dosages, and symptoms. For example, a sentence like “Patient reports shortness of breath and is taking 500mg metformin twice daily” would surface the condition, medication, and dosage as structured fields.
- Contextual classification
Recognized terms are linked to standardized coding systems such as ICD-10, SNOMED CT, or LOINC. This ensures interoperability with EHRs and supports analytics use cases like chronic disease management and patient risk stratification.
- Relationship mapping
Beyond simple tagging, advanced NLP can infer relationships such as whether a medication is prescribed or discontinued, or whether a symptom is current, historical, or hypothetical. This contextualization is vital for accurate predictive modeling.
- Integration into healthcare data analytics platforms
Once structured, the information flows into dashboards, population health tools, and clinical decision support systems. Physicians can then view patient trends over time, compare against population cohorts, or trigger alerts when values exceed thresholds.
Why Interpreting Clinical Conversations Matters
AI clinical documentation reduces the burden of manual data entry, freeing clinicians to focus more on patient interaction. More importantly, it establishes a consistent, machine-readable foundation for healthcare business intelligence. When thousands of individual encounters are structured in this way, organizations can:
- Detect emerging population health trends earlier
- Support epidemiological data analysis with richer datasets
- Improve predictive healthcare modeling accuracy
- Generate mental health and telehealth insights from conversations that were previously inaccessible to analytics
Therefore, NLP acts as the bridge between human dialogue and machine intelligence, ensuring that the richness of clinical conversations is not lost but converted into actionable intelligence.
III. Applications Across Care Settings
Turning clinical conversations into structured insights directly shapes how care is delivered across different healthcare environments. By embedding NLP and AI into healthcare data analytics platforms, organizations can shift from reactive documentation to proactive intelligence that supports clinicians, patients, and administrators alike.
Below are four key areas where these capabilities are already showing tangible impact:
Primary Care
Structured notes give physicians a clearer view of patient history and trends, enabling early detection of risk factors and preventive action.
Specialty Clinics
In areas like cardiology or endocrinology, structured data supports continuous monitoring and timely care adjustments for chronic diseases.
Telemedicine
An AI-powered telehealth analytics platform can transcribe and organize virtual visits into standardized records for billing, compliance, and quality tracking.
Behavioral Health
NLP captures patterns in mood and therapy progress from unstructured notes while maintaining HIPAA compliance .
Emergency and Acute Care
Real-time data and NLP-analyzed notes help flag high-risk patients and improve coordination during critical interventions.
Together, these capabilities reduce administrative overhead, strengthen decision support, and create a consistent data foundation for system-wide performance improvement.
IV. Building a Healthcare Data Analytics Platform That Lasts
Technology choices determine whether a clinical data analytics platform can scale, remain compliant, and deliver insights clinicians actually use. The goal is not just to capture data but to create a foundation that is secure, interoperable, and adaptable as care models evolve.
Below are core capabilities that healthcare leaders should prioritize when designing or modernizing their platforms:
| Capability | Value for Healthcare | When to Prioritize |
|---|---|---|
| Cloud-based medical analytics | Scalability and integration across sites | Early, to avoid siloed systems |
| HIPAA-compliant analytics platform | Security, auditability, and regulatory alignment | Non-negotiable at launch |
| Medical imaging analytics AI | Structured insights from scans | Secondary, as imaging requires specialized models |
| Real-time patient data monitoring | Immediate alerts and care adjustments | Essential for critical care units |
| Telehealth analytics integration | Structured documentation from virtual visits | As telehealth volume scales |
Taken together, these technological capabilities form the backbone of a modern healthcare business intelligence ecosystem. A cloud-first, compliance-ready foundation ensures security and interoperability, while layered capabilities, such as imaging and telehealth analytics, add specialized insights as the platform matures.
V. Building Trust and Driving Measurable Impact With AI-Driven Clinical Documentation
AI-driven documentation can only succeed if it earns clinician trust while delivering tangible business value. Adoption hinges on two critical dimensions: compliance and usability on one side, and measurable improvements in efficiency and outcomes on the other.
Compliance and Trust
Clinicians need confidence that new systems safeguard patient data and align with their workflows. That means:
- Meeting HIPAA and GDPR standards for patient privacy
- Providing full audit trails for every access event
- Delivering explainable outputs that clinicians can validate
- Integrating seamlessly into existing EHR environments
Business and Clinical Value
Physicians are already embracing AI in their work. An AMA survey found that two out of three physicians used healthcare AI in 2024, particularly for documenting billing codes, medical charts, discharge instructions, care plans, and even translation or assistive diagnosis tasks [5].
When AI reduces repetitive documentation, organizations gain more than efficiency:
- Greater clinician satisfaction and reduced burnout
- Faster billing and claims turnaround
- Richer, more structured datasets for analytics and research
- Lower costs tied to medical errors and readmission prevention
The ROI extends beyond operational savings. By pairing trust with measurable impact, healthcare business intelligence platforms position organizations for stronger performance in value-based care environments.
VI. Turning Documentation Burden into Strategic Advantage :
Once the case for structured documentation is established, execution requires a partner that can translate vision into outcomes. Matellio builds custom healthcare solutions that do more than capture information by :
- Converting unstructured notes and conversations into analytics-ready data
- Providing HIPAA-compliant architectures with real-time monitoring and audit trails
- Integrating chronic disease analytics, predictive healthcare modeling, and community health insights
- Reducing clinician burden with intuitive AI-driven interfaces
By enabling this shift, Matellio helps healthcare organizations move from documentation-heavy workflows to actionable intelligence that accelerates funding, adoption, and patient trust.
One example of this impact can be seen in Matellio’s work with Neurosens, a healthcare provider that sought to eliminate inefficiencies in clinical documentation.
Case Study:
Automating Referral Letters for Neurosens
The Challenge
Neurosens faced significant inefficiencies in clinical documentation. Physicians were spending excessive time manually drafting referral letters, resulting in delays, errors, and administrative strain.
The absence of standardized practices compounded the issue, while siloed systems limited collaboration across care teams and slowed patient transitions. Neurosens needed an AI-powered platform that could improve speed, accuracy, and compliance without adding complexity to clinicians’ workflows.
The Solution
Matellio partnered with Neurosens to develop ClinicalPad, a web-based platform that automates referral letter generation directly from clinical notes.
Using Generative AI and machine learning, ClinicalPad removes the need for manual data entry, introduces customizable templates, and provides real-time editing and preview functions for clinicians and administrators alike. Secure two-step authentication and encryption ensure regulatory compliance, while integrated print and email options streamline distribution.
The Results
- Referral letter creation dropped from 15 minutes to just seconds
- Letters became more accurate and consistent
- Manual entry errors were removed entirely
- Clinicians and staff collaborated more smoothly
- Patient handoffs and transitions moved faster
- All data stayed secure under HIPAA standards
This project shows how Matellio turned a time-consuming documentation process into a faster, more accurate, and secure system, giving clinicians more time for patients. The Neurosens success story also shows how AI-powered documentation can be applied in many areas of care, not just referrals.
VII. Advancing Clinical Documentation with A
The future of healthcare documentation is about making every patient conversation count. By using NLP to turn spoken or written notes into structured data, healthcare providers can cut down on repetitive paperwork, keep records secure, strengthen compliance, and generate insights that improve care.
With the right tools and a custom healthcare solutions partner like Matellio, the move from scattered notes to meaningful intelligence is now practical and achievable.
Healthcare leaders can’t afford to wait. Don’t wait to fall behind.
Reduce costs, strengthen compliance, and position your organization for data-driven growth in a competitive market.
Ready to modernize your systems?
See how the right enterprise tech partner can accelerate your growth.
Key Takeaways
- Tapping the hidden data goldmine: 97% of healthcare data goes unused, but AI platforms can change that.
- Structuring conversations into insights: NLP transforms clinical dialogue into analytics-ready, reliable data.
- Driving outcomes across care settings: Predictive risk stratification, chronic disease analytics, telehealth, and mental health all see measurable benefits.
- Making adoption sustainable: Trust, compliance, and seamless usability matter just as much as technical accuracy.
- Building a future-ready analytics foundation: Cloud-first, secure, and interoperable platforms set the stage for long-term scalability.
FAQ’s
By structuring patient data, analytics platforms highlight trends, compare outcomes, and surface best practices. Thus, physicians gain decision-support tools that complement their clinical judgment.
Medication errors, adverse events, readmission rates, and real-time vitals are critical. Structured data makes tracking these metrics more reliable and accurate.
Yes, predictive healthcare modeling can combine vital signs, laboratory results, and NLP-analyzed notes to identify high-risk patients for rapid intervention.
Structured platforms audit prescribing patterns, alert clinicians to potential contraindications, and identify anomalies in real-time. error.
Patterns in disease progression, treatment adherence, and population-level health trends can be identified once unstructured notes are standardized and organized.
Patient feedback, wait times, and care outcomes can be monitored and analyzed to guide service improvements.
HIPAA-compliant platforms feature role-based access control and comprehensive audit logs to track who accesses data and when.
Start with foundational elements that include HIPAA compliance, real-time monitoring, and predictive modeling. Then layer in specialized tools, such as imaging AI or telehealth analytics.
References:
[1] World Economic Forum, 4 ways data is improving healthcare
[2], [3] McKinsey, Unlocking peak operational performance in clinical development with artificial intelligence
[4] Grand View Research, Healthcare Business Intelligence Market (2025 – 2033)
[5] AMA, 2 in 3 physicians are using health AI—up 78% from 2023


