Executive Summary
Clinicians in the United States spend approximately 13 hours per week on documentation and indirect patient care tasks—time that could be devoted to treating patients [1]. Every lab report trapped in a silo, every duplicated note, and every delayed update adds friction to care delivery. The result is mounting administrative fatigue, operational waste, and fragmented treatment decisions that compromise patient care quality.
Despite efforts to modernize, full interoperability is still out of reach. In 2023, about 70% of non-federal U.S. acute care hospitals could send, find, receive, and integrate patient data, leaving nearly one-third still operating in silos [2].
The healthcare sector’s ability to deliver high-quality, efficient care now depends on how fast it can turn information chaos into coordinated insight. AI-powered EHR integration is emerging as the turning point, merging documentation, analytics, and real-time decision support into a single, adaptive workflow.
Modern frameworks, such as SMART-on-FHIR integration, enable secure interoperability between EHRs and third-party AI applications. The discussion ahead outlines how AI-integrated EHR systems are helping healthcare leaders streamline operations, improve clinical accuracy, and advance the shift toward intelligent care delivery.
Matellio stands at the forefront of this transformation, partnering with healthcare organizations to design and implement AI-driven EHR/EMR solutions that address these challenges head-on. With deep expertise in HIPAA-compliant architecture, FHIR R4 standards, and custom AI integration, Matellio transforms fragmented systems into unified, intelligent workflows. Our approach combines technical precision with clinical usability, ensuring that every solution not only meets regulatory requirements but also delivers measurable improvements in care coordination, documentation accuracy, and operational efficiency. Whether you’re looking to eliminate data silos, reduce administrative burden, or accelerate your digital transformation, Matellio provides the roadmap and execution capability to turn your vision into reality.”
I. EHR Integration as the Foundation of Intelligent Clinical Workflows
Integration today is about aligning data, intelligence, and workflow. In traditional setups, clinicians navigate between multiple interfaces for lab results, imaging data, and patient histories. Each platform requires manual input, which leads to transcription errors and fragmented records.
A fully integrated EHR environment changes this dynamic. It consolidates structured and unstructured data, from clinical workflow automation to device feeds, into a unified layer accessible across departments.
When combined with AI models trained for clinical context, this foundation transforms static recordkeeping into dynamic decision support. The process strengthens coordination across specialties, reduces redundant documentation, and improves visibility into each stage of patient care.
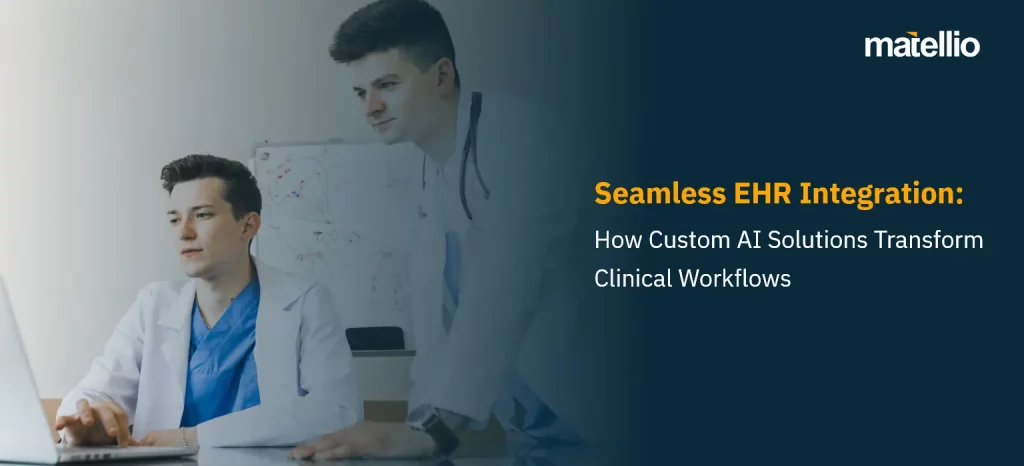
Advantages of AI EHR Integration in Value-Based Healthcare Settings
- Improved Data Accessibility: Clinicians can instantly retrieve lab results, imaging reports, and patient histories from one interface, reducing delays in diagnosis and treatment.
- Fewer Documentation Errors: Automated data entry and synchronization reduce transcription mistakes and missing information.
Studies show that EHR systems significantly reduce medical error rates, with one comprehensive analysis finding that properly implemented EHR systems improve operational effectiveness and reduce error rates immediately [5]. Healthcare organizations implementing advanced EHR technologies have reported reducing medication errors by up to 27% through integrated decision support systems [6].
- Enhanced Clinical Decision Support: AI-driven EHR systems surface relevant patient data and treatment options in real time, improving care accuracy.
Research demonstrates that diagnostic accuracy increased by 4.4 percentage points when clinicians were provided with AI model predictions and explanations during complex diagnostic scenarios [7]. Furthermore, AI-backed diagnostic support has been shown to reduce error rates by up to 30% in complex diagnostic cases [8].
- Streamlined Workflows: Integrated systems eliminate repetitive data entry and manual reconciliation between departments.
AI-powered documentation tools can reduce physician documentation time by 20% to 30%, translating to approximately 1 hour less time spent documenting per week for high-support physicians [9]. One health system reported saving 15,791 hours of documentation time using AI scribes over one year [10].
- Better Care Coordination: Multiple specialists can access and update the same patient record, ensuring continuity of care.
Research shows that patient-reported care coordination is strongly associated with better clinical outcomes, with coordinated care environments demonstrating measurable improvements in patient safety metrics [11].
- Cost Efficiency: Avoiding duplicate tests and redundant procedures saves operational costs.
Duplicate patient records account for approximately 22% of all records in some hospital systems, resulting in $96 in additional costs per duplicate [12]. Moreover, health information exchange use has been associated with cost savings of nearly $2,000 per patient, largely due to reduction in unnecessary testing [13]. The U.S. healthcare system could save over $30 billion annually by improving medical device and EHR interoperability [14].
- Higher Patient Satisfaction: Faster consultations, accurate records, and fewer repeat diagnostics lead to better overall patient experiences.
Studies indicate that EHR integration significantly enhances patient engagement, with 63% of physicians agreeing that EHRs have led to improved patient care [15].
Every redundant test avoided and every minute saved on documentation directly improves operational margins and patient outcomes. For hospital groups and multi-specialty networks, integration drives not just clinical improvement but measurable ROI through optimized throughput and reduced administrative overhead.
II. Why Integration and AI Acceleration Have Become Strategic Priorities
The need for interoperability has grown urgent. Despite years of EHR adoption, only 30% of U.S. providers [3] report achieving full interoperability. Data remains isolated between labs, pharmacies, and remote monitoring systems. This fragmentation limits accurate diagnostics, complicates chronic care management, and erodes the quality of clinical decision-making.
Regulatory frameworks now push toward standardization. The ONC’s interoperability mandates and the adoption of FHIR and SMART-on-FHIR EHR APIs have accelerated data exchange capabilities. In 2022 alone, over two-thirds of non-federal acute care hospitals have adopted FHIR APIs, and nearly 90% use secure API connectivity [4] to facilitate real-time data sharing.
Artificial intelligence is now being positioned as the layer that transforms compliance-driven data collection into proactive, intelligence-driven workflow optimization. It enables clinicians to document, analyze, and act faster through embedded intelligence within their familiar systems.
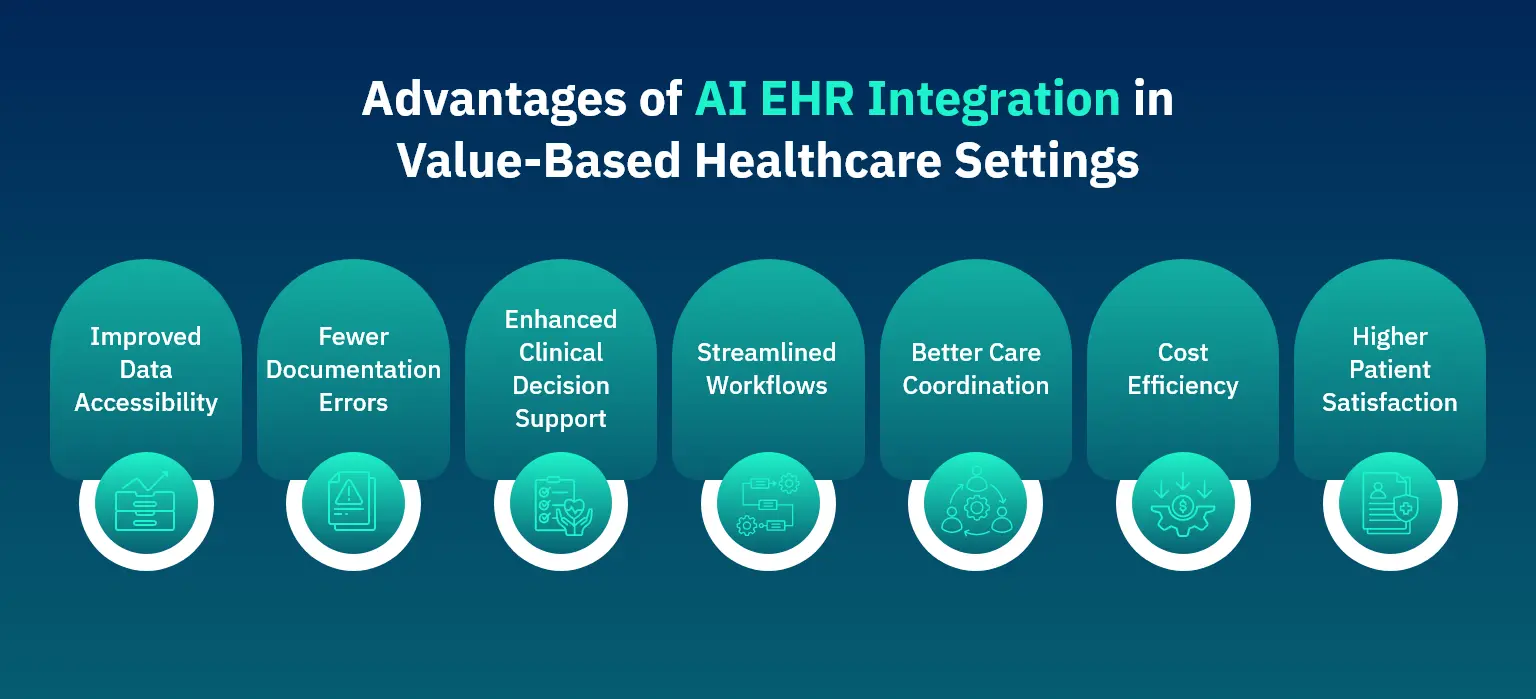
The Core Enablers of AI-Driven EHR/EMR Integration
A strong integration strategy combines five capabilities that reinforce data quality, security, and clinician efficiency. Each capability is part of an ecosystem, a continuum that moves healthcare from reactive administration to predictive, coordinated care.
Unified Data Aggregation and Normalization
AI-powered integration consolidates structured data from EHR fields, unstructured data from physician notes, and continuous streams from IoT or wearable devices. Once standardized, this unified dataset enables analytics to operate consistently across use cases. It reduces duplicate testing and allows AI models to build more accurate patient profiles for early intervention.
AI-Enhanced Documentation within Workflows
Intelligent voice recognition and NLP-based ‘AI scribes’ transcribe and structure clinician-patient conversations in real time. This reduces manual entry errors and improves the accuracy of clinical documentation. AI-based clinical documentation tools have demonstrated accuracy rates as high as 92% when extracting and structuring clinical data [16]. Studies show that AI documentation automation can reduce documentation time by 56% in some implementations [17].
API-Centric and Standards-Based Connectivity
Open standards such as SMART-on-FHIR, OAuth 2.0, and RESTful APIs enable secure data exchange between EHRs and AI applications without custom middleware. This architecture supports scalable interoperability across vendors, allowing the hospitals to introduce new digital tools without complex reengineering.
Real-Time Analytics and Decision Support
Integrated AI models monitor patient data in real time, flagging anomalies and recommending timely interventions. The diagnostic delay is significantly reduced when real-time CDS is used in clinical trials. These tools support faster decision-making and measurable improvements in patient safety.
Compliance and Data Governance
Security remains non-negotiable. Robust integration frameworks enforce encryption, access controls, and detailed audit trails. Adherence to HIPAA compliance in healthcare and GDPR standards ensures patient trust and institutional accountability. Data governance models further guarantee that every transaction is tracked, validated, and compliant.
III. How Custom AI Healthcare Solutions Strengthen Accuracy and Productivity
Off-the-shelf models may generalize insights, but custom AI healthcare solutions trained on a provider’s own data improve prediction accuracy and reduce false alerts. They learn from real-world patterns (clinical language, documentation habits, and population demographics), ensuring that every recommendation is relevant.
Custom AI also relieves pressure on teams with clinical workflow automation. Its automated transcription, context-aware field completion, and real-time summarization free physicians from routine tasks.
The impact of custom AI on clinical accuracy is significant. Research demonstrates that AI clinical decision support can improve diagnostic accuracy from baseline levels of 73% to 77.5% when AI predictions are combined with explanations [7]. In another study examining AI’s impact on reducing diagnostic errors, error rates decreased from 22% to 12% after AI integration, representing a 45% reduction in diagnostic errors [18].
Documentation quality and efficiency improvements are equally compelling. Studies show that AI-powered tools can structure clinical data with F-scores ranging from 0.86 to 0.92, indicating high accuracy in extracting and organizing clinical information [19]. More importantly, physicians using ambient AI documentation assistants experienced a 21% decrease in time spent writing notes, freeing up approximately one hour per week for direct patient care [20].”
The focus is on simplifying the decision-making while technology fits around human expertise rather than the other way around.
SMART-on-FHIR Drives Scalable Interoperability
Healthcare interoperability has long struggled with inconsistent standards and proprietary architectures. SMART-on-FHIR integration addresses these limitations by providing a universal framework for building and connecting healthcare applications.
The SMART solution stands for Substitutable Medical Applications and Reusable Technologies. It combines the FHIR data model with OAuth 2.0-based security to manage authorization between EHRs and external applications. This model allows hospitals to deploy AI solutions that access patient data securely, analyze it, and provide insights into existing workflows. Its components are:
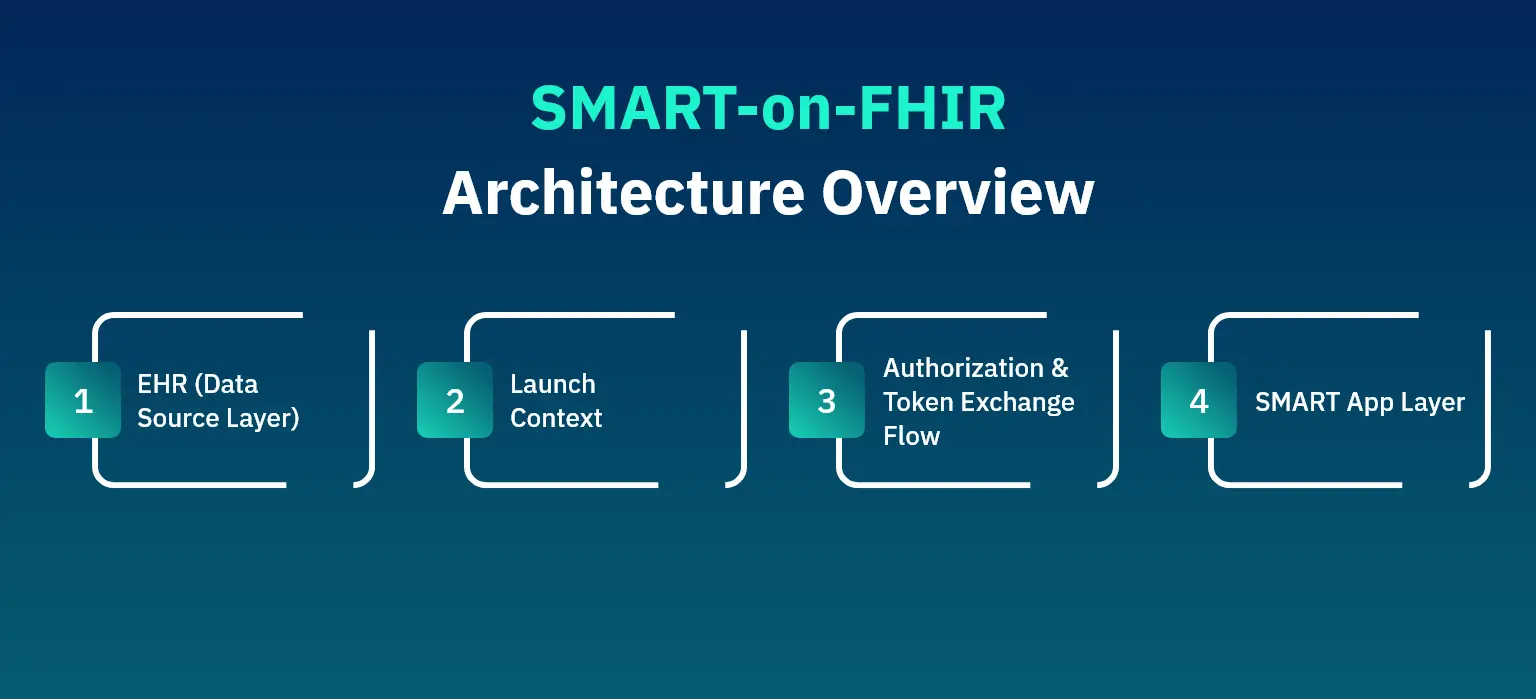
SMART-on-FHIR Architecture Overview
| Layer/Component | Key Functions and Description |
| EHR (Data Source Layer) |
|
| Launch Context |
|
| Authorization and Token Exchange Flow |
|
| SMART App Layer |
|
The benefits extend across stakeholders.
- For developers, SMART-on-FHIR EHR API accelerates deployment and reduces integration costs.
- For providers, it delivers interoperability without vendor lock-in.
- Lastly, for patients, it enables a consistent experience as their data follows them across care settings.
IV. How Matellio Supports AI-Driven EHR/EMR Integration
Matellio builds scalable, HIPAA-compliant EHR and EMR solutions that connect data, analytics, and clinical workflows into a unified ecosystem. Our expertise spans EHR software and app development, API-based integration, and advanced analytics, all designed to make healthcare data more accessible, actionable, and secure.
Each engagement starts with assessing existing systems and workflows. Using FHIR R4, SMART-on-FHIR, and other open standards, Matellio designs secure interoperability blueprints that connect EHRs, third-party apps, and IoT-enabled devices. The outcome is a modular, AI-ready environment that supports:
- Automated documentation and scheduling
- Predictive analytics for clinical and operational insights
- Seamless integration with billing, telehealth, and RCM platforms
Matellio’s co-development model aligns technical precision with clinical usability, ensuring every solution is secure, scalable, and compliant with HIPAA, GDPR, and ONC standards.
As part of our healthcare modernization projects, Matellio has enabled hospitals and care networks to enhance collaboration, reduce administrative friction, and accelerate patient throughput. The following case study highlights how these capabilities translate into measurable impact for healthcare providers.
Optimizing Discharge Workflows for Healthcare Providers
Challenges
Hospitals and skilled nursing facilities faced fragmented discharge processes managed through spreadsheets and emails. This manual approach caused delays, miscommunication, and compliance risks. Coordinating with hospice and care providers became time-consuming, affecting patient transitions and overall quality of care.
Solution
Matellio developed MaxMRJ, a HIPAA-compliant discharge planning system that automates coordination, accelerates discharges, and enhances collaboration. The platform aggregates patient data, integrates with EMRs, and enables real-time communication between hospitals and care providers.
By automating referrals, documentation, and task tracking, MaxMRJ eliminated inefficiencies and ensured seamless patient transitions.
Outcomes
- Streamlined discharge workflows
- Optimized referral network efficiency
- Enhanced compliance and data security
- Faster patient discharge processing
- Improved coordination across facilities
- Automated documentation and task tracking
V. The Future of Intelligent Care Systems
AI in healthcare operations is evolving toward continuous intelligence, where data from every interaction informs real-time decisions. Ambient AI scribes, predictive diagnostics, and connected monitoring tools are shaping the next generation of clinical workflows. As interoperability improves, AI models become more precise, and the demand for clean, shareable data grows in parallel.
The impact of AI-EHR integration will soon be defined not by connectivity alone but by how well it orchestrates the entire patient journey. Systems that unify insights from wearables, home diagnostics, and genomic data into clear, actionable intelligence will set new standards for care delivery. Healthcare leaders who invest now will be positioned to lead the era of data-driven, predictive care.
Key Takeaways
- AI-Driven Integration: EHR and EMR integration powered by AI drives efficiency, precision, and value-based healthcare outcomes.
- SMART-on-FHIR for Interoperability: Open standards such as the SMART-on-FHIR EHR API ensure seamless data exchange, scalability, and vendor-neutral connectivity.
- Custom AI for Clinical Accuracy: Tailored AI models improve documentation quality, reduce clinician burden, and support better patient decisions.
- Compliance-First Innovation: Strict adherence to GDPR, ONC, and HIPAA compliance in healthcare safeguards patient data, strengthens institutional trust, and lays a secure foundation for scalable digital transformation in healthcare.
- Matellio as a Co-Creation Partner: Partnering with technology experts like Matellio ensures co-created, future-ready healthcare ecosystems built for longevity and trust.
FAQ’s
AI automates repetitive documentation, prioritizes relevant patient insights, and provides real-time recommendations that reduce manual input and cognitive load.
AI-driven tools improve data accuracy, speed up decision-making, minimize duplication, and enhance operational efficiency while maintaining compliance.
Custom AI healthcare solutions models trained on institutional data normalize inconsistent records, auto-populate documentation fields, and minimize repetitive entry, freeing clinicians to focus on patient interaction.
Encryption, audit logging, access control, and early regulatory involvement are essential. Secure APIs such as OAuth 2.0 and data minimization ensure compliant data exchange.
SMART-on-FHIR integration applies a consistent data model and authentication framework that allows authorized applications to interact safely with EHR data across multiple systems.
References:
[1] American Medical Association, Doctors work fewer hours, but the EHR still follows them home https://www.ama-assn.org/practice-management/physician-health/doctors-work-fewer-hours-ehr-still-follows-them-home
[2] National Library of Medicine, Interoperable Exchange of Patient Health Information Among U.S. Hospitals: 2023
[3] Market.us Media, Electronic Health Records Statistics 2025 By Healthcare, Data, Management
[4] American Medical Association, Doctors work fewer hours, but the EHR still follows them home https://www.ama-assn.org/practice-management/physician-health/doctors-work-fewer-hours-ehr-still-follows-them-home
[5] National Library of Medicine, The Effects of Electronic Health Records on Medical Error Reduction https://pmc.ncbi.nlm.nih.gov/articles/PMC11525084/
[6] BMC Nursing, The effect of electronic medical records on medication errors and patient safety https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-024-01936-7
[7] JAMA Network, Measuring the Impact of AI in the Diagnosis of Hospitalized Patients: A Randomized Clinical Vignette Survey Study https://jamanetwork.com/journals/jama/fullarticle/2812908
[8] Rocket Doctor AI, How AI Enhances Diagnostic Accuracy in Clinical Decision Support https://www.rocketdoctor.ai/blogs/how-ai-enhances-diagnostic-accuracy-in-clinical-decision-support/
[9] JAMA Network, Physician EHR Time and Visit Volume Following Adoption of Team Documentation https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2822382
[10] American Medical Association, AI scribes save 15000 hours—and restore the human side of medicine https://www.ama-assn.org/practice-management/digital-health/ai-scribes-save-15000-hours-and-restore-human-side-medicine
[11] National Library of Medicine, Patient-Reported Care Coordination is Associated with Better Outcomes https://pmc.ncbi.nlm.nih.gov/articles/PMC8642573/
[12] HFMA, Hidden Costs of Duplicate Patient Records https://www.hfma.org/operations-management/cost-reduction/60322/
[13] California Health Care Foundation, Health Data Exchange Drives Efficiency and Cuts Costs https://www.chcf.org/resource/health-data-exchange-drives-efficiency-cuts-costs/
[14] West Health Institute / Helixbeat, The True Cost Of Fragmented Healthcare Data https://helixbeat.com/the-true-cost-of-fragmented-healthcare-data/
[15] Stanford Medicine, How Doctors Feel About Electronic Health Records – National Physician Poll https://med.stanford.edu/content/dam/sm/ehr/documents/EHR-Poll-Presentation.pdf
[16] National Library of Medicine, Improving Clinical Documentation with Artificial Intelligence: A Systematic Review https://pmc.ncbi.nlm.nih.gov/articles/PMC11605373/
[17] National Library of Medicine, Speech-recognition based EMR with 97% accuracy https://pmc.ncbi.nlm.nih.gov/articles/PMC11605373/
[18] Healthcare Bulletin UK, Artificial Intelligence in Internal Medicine: A Study on Reducing Diagnostic Errors and Enhancing Efficiency https://healthcare-bulletin.co.uk/article/artificial-intelligence-in-internal-medicine-a-study-on-reducing-diagnostic-errors-and-enhancing-efficiency-4148/
[19] National Library of Medicine, Deep learning applied to extracting social determinants of health with high accuracy (F-score 0.86-0.92) https://pmc.ncbi.nlm.nih.gov/articles/PMC11605373/
[20] JAMA Internal Medicine, Team-based documentation reduced physician documentation time by 21% https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2822382